BREAST BIOPSY AUSTIN
In a breast biopsy, tissue is taken from the breast and examined under the microscope (usually) to determine whether or not cancer is present. Basically there are 2 techniques: Fine needle aspiration (FNA), image-guided core needle biopsy, excisional biopsy, incisional biopsy. Get the best breast biopsy Austin has to offer with Dr. Miltenburg and her expert team at Breast Health Institute Austin.
FNA
Fine needle aspiration (FNA) is the least invasive biopsy technique. It is often used when the doctor suspects a cyst (see “There is something wrong with my breast”) or to biopsy a lymph node. The problem with FNA is if malignant cells are seen, the pathologist may not be ale to tell if the cancer is invasive or non invasive. This distinction is very important because it guides treatment decisions. So if cancer is diagnosed on FNA, additional biopsies may be necessary.
Needle Core Biopsy for Breast
This technique is used when an abnormality is seen on breast imaging such as mammogram, ultrasound or MRI. If mammogram is used to guide the breast biopsy it’s called a stereotactic biopsy. Otherwise it is called an ultrasound-guided core needle biopsyor MRI-guided core needle biopsy. The procedure is usually done by a radiologist but can also be performed by a surgeon.
The skin is cleansed and the area is usually (but not always) anesthetized with local anesthetic. A small nick is made in the skin with a scalpel;a needle is inserted into the area of concern and several very small cores of tissue at removed. The doctor will take 3 cores or more, as many as necessary to be confident about the pathology results.
Needle Core Biopsy Instructions for Patients
Relax,needle core breast biopsies procedures are common and most patients tolerate them very well.
How to prepare
- Shower and wash your entire body with Dial soap the day before the biopsy and the morning of the biopsy.
- Do not wear deodorants, antiperspirants or talcum powder on the day of biopsy because most of these products contain aluminum particles which look like tiny white dots on mammogram and appear similar to the calcification’s seen in some breast cancers.
- Do not take aspirin or non-steroidal anti-inflammatory drugs (NSAIDs) for 7 days before the biopsy because these drugs affect bleeding. It is OK to take Tylenol.Aspirin and NSAIDs can be resumed one day after the procedure.
- Get to your appointment on time. Allow extra time for traffic, parking, etc.
- Wear a bra that ties up in the front or the back but does not go on over the head.
- Wear a shirt that buttons up in the front.
- Leave valuables at home but bring identification (I.D.) and insurance information
- Someone should drive you home
- The radiologist will want to review outside films in preparation for the biopsy so if you have images such as mammograms, ultrasounds, MRI from another facility be sure the place doing the biopsy has them before the biopsy day. You may have to pick them up and deliver them yourself.
What to expect on biopsy day
- You should receive detailed information from the facility
- Plan to be there for at least 4 hours
- You will be awake for the procedure
- The radiologistwill numb the area with local anesthetic. You can ask for more if you feel discomfort.
- Several tiny pieces of tissue will be taken
- A clip/tissue marker will be placed after the biopsy to mark the biopsy site and a mammogram will be done to confirm the clip position
- Sometimes there is bleeding but it’s not a lot and it can usually be controlled by holding pressure.
Care after biopsy
- Wear a supportive bra 24/7 on the day of biopsy and the following day. After that you can just wear a bra during the day.
- There will be a dressing on the biopsy site. As a general rule you leave it on until it comes off on its own.
- Apply an ice pack to the area for 24 hours after the biopsy.
- You may shower, drive and return to work the day after biopsy.
- There may be bruising and/or swelling. Ice can help prevent or minimize this.
- Biopsy results take about 5 business day. Make sure you know how you are going to get the pathology results: follow up appointment in the office, phone call, etc.
- For possible pathology results see Pathology Report
What do you see when you look inside the breast?
Did you ever wonder what the inside of a breast looks like? This is a photo I took in the operating room. It captures some of the main components that make up the human female breast. As you can see, the incision was made around the lateral (outer) side of the areola of the left breast and the dissection proceeded through the subcutaneous fat. The breast itself is just deep to the subcutaneous fat.

The breast is made up of several elements (See Something’s wrong with my breasts). Mammary gland tissue is the component that makes milk. Itis white in color and often very firm or dense (kind of like the inside of a raw potato). The mammary gland is made up of lobules (lobules contain alveoli which make the milk) and ducts (which carry the milk out to the nipple). These two elements are not discernable to the human eye. In other words, you cannot tell them apart in the operating room. They can only be seen with a microscope. In 90% of cases, breast cancer begins when the cells that line the milk ducts mutate and become malignant (ductal carcinoma). In 10% of cases, cancer begins when the cells that line the lobules turn malignant (lobular carcinoma).
The small milk ducts in the mammary gland converge into 10 – 12 major lactiferous ducts that leave the mammary gland and enter the nipple (see diagram).
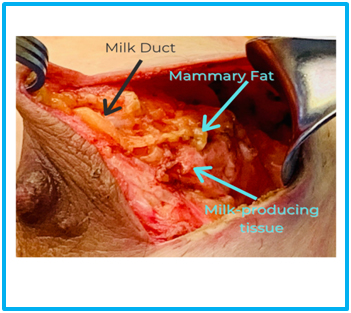
Distributed randomly around and through the milk-producing tissue in mammary fat which is yellow in color and soft. Fat is pretty easy to tell apart from glandular tissue. Breasts also have connective tissue which gives the breast its shape. It is the connective tissue that gives rise to fibroadenomas which are benign tumors very common in young ladies (see fibroadenoma). Breasts also contain intramammary lymph nodes and occasionally patients develop lymphoma (cancer of the lymph nodes) in the breast.
Female hormones are responsible for the development and maintenance of mammary glandular tissue. In menopause, female hormone levels drop resulting in mammary gland regression or involution. In this natural process, the glandular breast tissue turns into fat. In general, postmenopausal women who do not take hormone replacement therapy have breasts that are mostly fatty replaced.
What does the breast look like after a lumpectomy?
The breast is quite forgiving. A skilled surgeon can remove quite a bit of tissue from the breast and once everything has healed the breast will not look smaller or dented or distorted. How can this be? When breast tissue is removed during lumpectomy a hole or space is left behind. Our bodies don’t like empty spaces so the body makes seroma fluid to fill the space. This is a normal physiological response. In other parts of the body, seromas can cause problems, but in the breast, a seroma is important to maintaining the shape, volume, and contour of the breast after a lumpectomy. Overtime (3-4 months) the body will absorb the seroma fluid and replace it with solid tissue. So, when the patient is naked and looks in the mirror, it looks like nothing happened. Sometimes you can feel an indentation or loss of volume in the area of a lumpectomy but you cannot see it. Of course, results vary but in my experience, most patients have an excellent cosmetic outcome.
Keep in mind that these results refer to patients who have a lumpectomy only. If, however, lumpectomy is followed by radiation the breast may look normal initially but over time it frequently becomes smaller and distorted. For the most part this due to the radiation. Whereas surgery heals over time, radiation decays but never completely goes away.
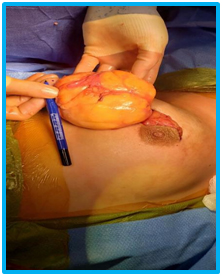
everything healed, the breast looked exactly the same.
Pathology Report
This is what I tell my patients: If the pathology shows cancer, well, you have cancer. But if the pathology is benign, we need to be 100% confident that the correct area was biopsied. Otherwise, we will have a false negative biopsy and that is a disaster.
A tiny titanium tissue marker (clip or chip) is placed in the area of the breast where the tissue was taken from. A mammogram is taken after the biopsy (post-biopsy mammogram) to document that the clip is in the correct position. Clip location should be recorded in the procedure note. Rarely, the clip is not in the correct position and when I tell patients that this can happen they are horrified. But it doesn’t panic! It doesn’t happen very often and even when it does it is not the end of the world (nothing is perfect). What’s important is that we know where the clip is in relation to the area of concern(that’s good medicine). We can take care of “malpositioned” clips.
The pathology report must be interpreted along with the procedure note.
The procedure note is only complete (signed off) when the doctor who performed the biopsy, in my practice it’s the radiologist, has reviewed the pathology report. That’s why it may take 6 or 7 days to get the official result. It’s not because the system is inefficient, it’s because quality work takes time. The radiology biopsy procedure note should comment whether the pathological diagnosis is concordant or discordant with the findings on imaging.
When results are concordant, the findings and recommendations are taken at face value.
Findings are discordant when the imaging and pathology don’t fit. An example of this is a BI-RADs 5 mammogram and a pathology report showing fragments of a fibroadenoma. In this instance the radiologist expected to find cancer but got a benign diagnosis. The scenario is discordant and the usual recommendation is surgical removal.

Checks to be sure a negative breast biopsy is a true negative and not a false negative:
- placement of post-biopsy tissue marker (clip)
- post-biopsy mammogram
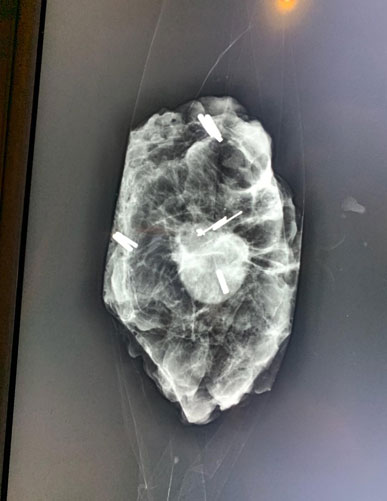
- specimen mammogram
- pathologist confirming placement of identifying features in tissue, such as localizing clip or calcifications or speculated mass
- 6 month follow up imaging (mammogram, ultrasound, MRI)
Excisional Biopsy
This may be referred to as anopen surgical biopsy.
An excisional biopsy / open surgical biopsy can done with or without localization.
Breast lesions that cannot be felt (palpated) on physical/clinical examination but are only seen on imaging need wire-localization. A very thin guide-wire is passed through the skin into area of concern. The patient is awake for this. After localization the patient is taken to the operating. An incision is made in the skin, the wire is followed to the mass or calcifications and the tissue is removed. Most of the time, the specimen is X-rayed to be sure the correct spot was removed. Then the tissue is sent to the pathologist for “biopsy”. The incision is sewn closed; the patient wakes up and goes home the same day. The surgery takes about 1 hour. Recovery is 2 to 3 days.
In cases where a breast mass is easy to feel, it can be surgically removed without localization. An incision is made and the mass is removed using special scissors or electro cautery or similar device. The tissue may or may not to X-rayed, depending on the circumstances. The tissue is sent to the pathologist for “biopsy”. The incision is sewn closed; the patient wakes up and goes home the same day. The surgery takes about 1 hour. Recovery is 2 to 3 days.
Excisional biopsy is very similar to lumpectomy / partial mastectomy. The difference is that in lumpectomy / partial mastectomy, the surgeon’s goal is to remove the lesion with a rim of surrounding normal tissue (margin). In an excisional biopsy, the intent is to remove the lesion only.
If the breast mass is large, only a part of the mass can removed. This is an open incisional biopsy.